Finding Clarity: Understanding The ALS Diagnosis Process
Receiving an ALS diagnosis, or even just wondering if you might have Amyotrophic Lateral Sclerosis, can feel like stepping into a very confusing space. It's a condition that touches the nerve cells responsible for movement, and figuring out what's going on can be a bit of a puzzle. This is because, as a matter of fact, the early signs of ALS can often look a lot like symptoms from other health issues, making the path to a clear diagnosis a thoughtful and thorough one.
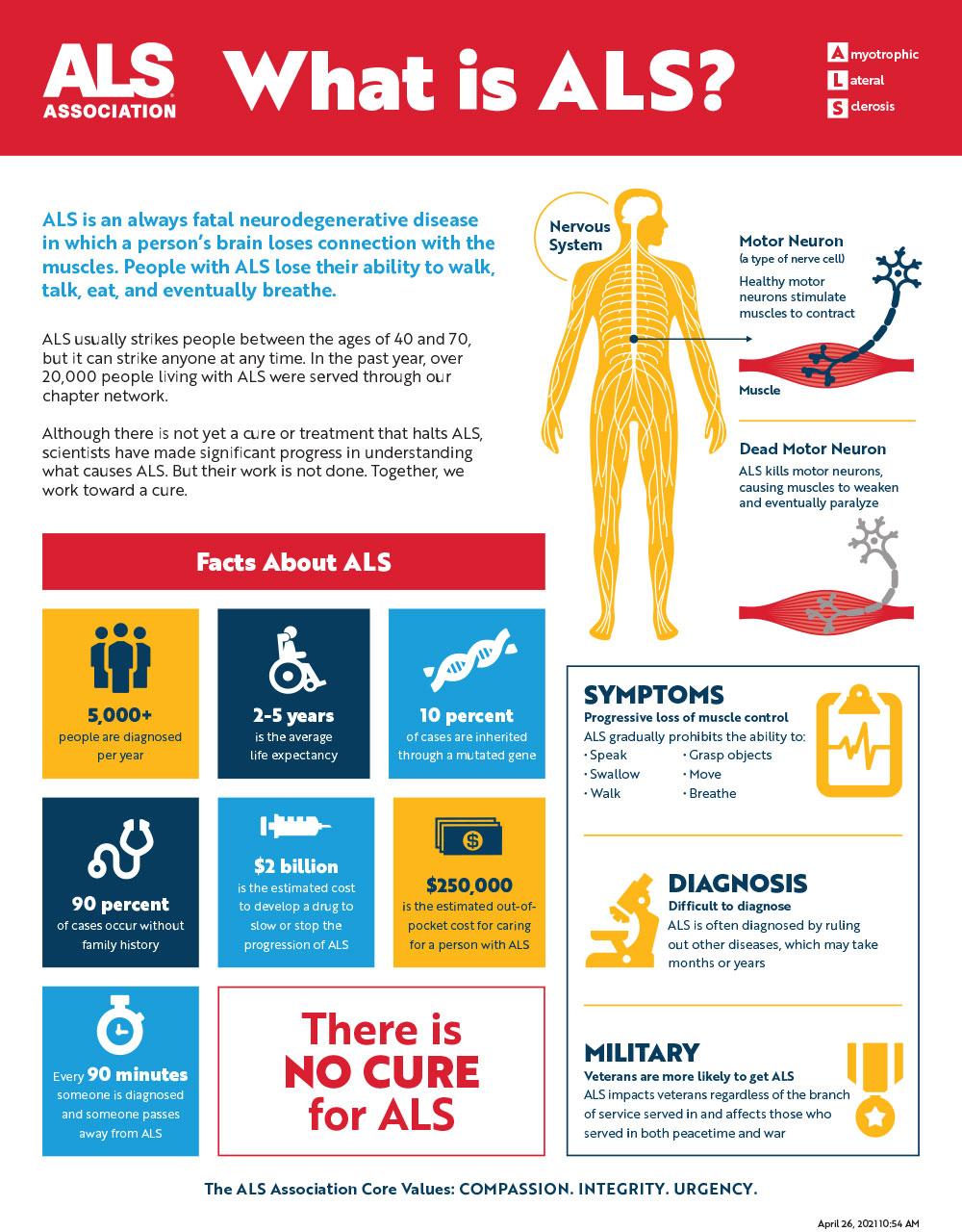
Amyotrophic Lateral Sclerosis, which many people also know as Lou Gehrig's disease, is a serious kind of neurological illness. It works by slowly wearing down the nerve cells in your brain and spinal cord—the very cells that tell your muscles what to do. This process, you know, leads to muscles losing their strength and control over time, which can really change how a person moves, speaks, and even breathes.
Because of how ALS starts and progresses, getting an accurate picture of what's happening inside the body is incredibly important. The journey to an ALS diagnosis is not always a quick one; it involves a careful look at a person's health, a series of tests, and the input from a team of medical experts. It's about ruling out other possibilities and, in a way, piecing together the evidence to confirm the presence of this specific motor neuron disease.
Table of Contents
- What is ALS and Why is Diagnosis Challenging?
- The Diagnostic Journey: A Team Effort
- Tests That Help Confirm an ALS Diagnosis
- The Progression of Symptoms
- Frequently Asked Questions About ALS Diagnosis
- Looking Ahead After Diagnosis
What is ALS and Why is Diagnosis Challenging?
Amyotrophic Lateral Sclerosis, or ALS, is a type of motor neuron disease that causes a progressive weakening of the muscles. It's a condition that, you know, affects the nerve cells in the brain and spinal cord that are responsible for sending messages to your muscles, telling them to move. Over time, these nerve cells become damaged, and the muscles they control start to lose their ability to work. This means that, very gradually, people with ALS find it harder to do everyday things that require muscle movement.
The Nature of ALS
ALS is considered a neurodegenerative condition. This means that it's a disease where the nerve cells, specifically the motor neurons, break down and die over time. These motor neurons are, in a way, the vital communication lines between your brain and your muscles. When they are damaged, the signals don't get through as they should, which leads to muscle weakness that just keeps getting worse. It's often called Lou Gehrig's disease, named after the famous baseball player who had it, and it is a fatal type of motor neuron disease, unfortunately.
The core issue in ALS is primary damage to these motor neurons. They are the ones that send the essential signals to the muscles that help us move. So, when these cells are not working correctly, the muscles don't receive the instructions they need, and they begin to waste away. This is why, you know, the condition leads to a loss of muscle control, which can impact almost every physical action someone performs.
- Symptoms Of Brain Tumor
- Christmas Movies At Netflix
- Liam Hemsworth
- Who Is The President In France
- Skibbidi Toilets
Early Signs and Their Variations
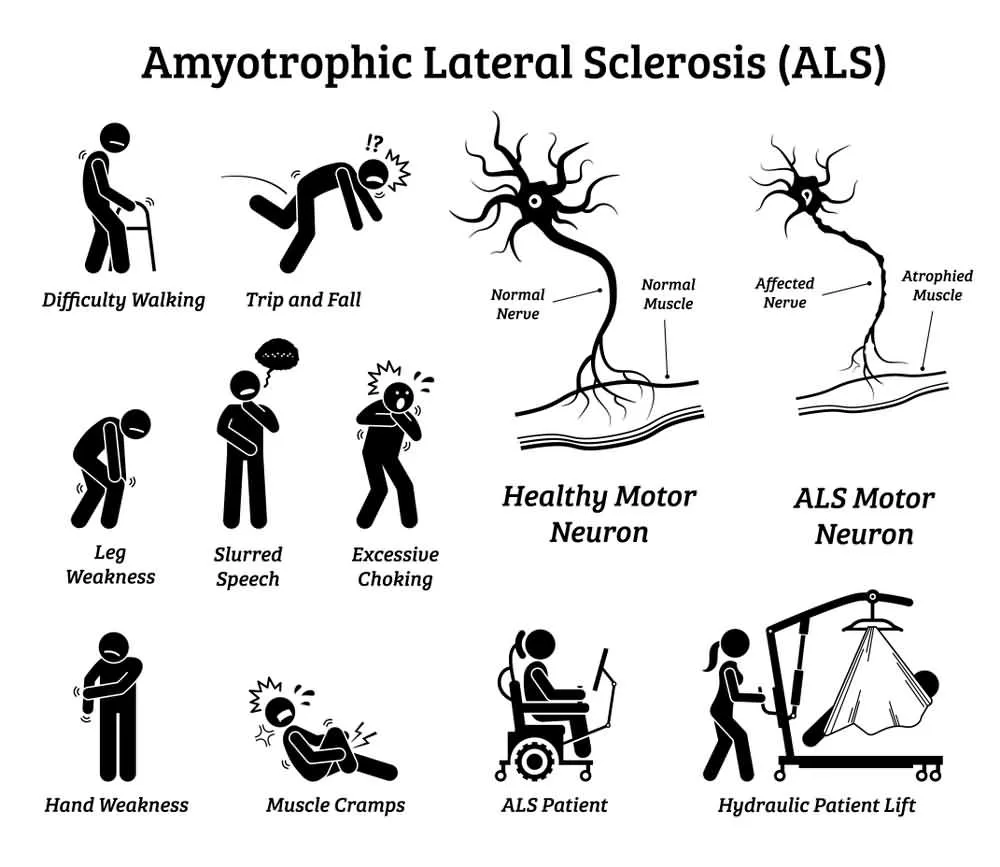
One of the main reasons why an ALS diagnosis can be a bit tricky to get early on is because its initial symptoms can be quite subtle and, frankly, mimic other less serious conditions. For instance, some people might first notice something like tripping more often, or perhaps they start dropping things they are holding. These early signs, it's almost like, they tend to affect your extremities, like your arms and legs, or sometimes even your breathing and eating functions right from the start.
Other early signs can vary quite a bit, but they might include things like muscle twitching, which is called fasciculations, or a feeling of weakness in a limb. For some, the first sign could be a slight change in their speech, perhaps it becomes a bit slurred. What I have is twitching, some people might say, and in ALS cases, let's say absolute initial, is the twitching. These initial symptoms are often what prompts someone to seek medical advice, which is a very important first step.
The Diagnostic Journey: A Team Effort
The path to an ALS diagnosis is not a straight line, and it very much involves a collaboration of medical professionals. It's a process of careful observation, detailed questioning, and a series of tests designed to either confirm ALS or rule out other potential causes for the symptoms a person is experiencing. This collaborative approach is, in a way, what helps ensure the most accurate outcome.
When to Seek Help
Often, the very first person to notice or hear about your ALS symptoms might be your primary care doctor. They are usually the first point of contact when you start experiencing unusual physical changes, like persistent muscle weakness or changes in speech. It's a good idea to bring up any concerns you have, even if they seem minor at first, because early observation can be helpful. Your primary care doctor, you know, plays a crucial role in directing you to the right specialists.
The Role of the Neurologist
Once your primary care doctor has an initial look, they will likely refer you to a doctor who has special training in nervous system diseases. This specialist is called a neurologist. Neurologists are the key players in the ALS diagnosis process because they have the specific knowledge and tools to evaluate conditions that affect the brain, spinal cord, and nerves. They will conduct thorough physical examinations and, you know, ask many detailed questions about your symptoms and medical history.
The neurologist's role is to assess your reflexes, muscle strength, coordination, and other neurological functions. They are looking for patterns of weakness and muscle changes that are characteristic of ALS. This initial evaluation by a neurologist is a very important step, as it helps guide which further tests might be needed to confirm or rule out the condition. They are, essentially, the experts who can distinguish ALS from other neurological disorders.
Comprehensive Care Groups
For people who are seeking a diagnosis or ongoing care for ALS, there are specialized groups that offer comprehensive support. These are often called ALS specialty groups, and they bring together a team of doctors and other healthcare professionals who focus specifically on this condition. People who seek diagnosis or treatment with the doctors of the Amyotrophic Lateral Sclerosis, also called ALS, specialty group receive comprehensive care. This means you get a coordinated approach to your health, which can be incredibly helpful.
These groups typically include neurologists, physical therapists, occupational therapists, speech therapists, dietitians, and social workers. Having such a team means that every aspect of your well-being can be addressed, from managing symptoms to getting support for daily living. It's a holistic approach, which is, you know, very beneficial for individuals and their families as they go through the diagnostic process and beyond.
Tests That Help Confirm an ALS Diagnosis
Because ALS can present with symptoms that look like other conditions, a big part of the diagnostic process involves performing various tests. These tests serve two main purposes: to rule out other diseases that might be causing similar symptoms and to gather evidence that points specifically to ALS. It's a bit like being a detective, gathering clues to solve a mystery, so to speak.
Ruling Out Other Conditions
One of the first things doctors will do is order tests to rule out other conditions. This is a very important step because many other neurological or muscular disorders can have symptoms that overlap with ALS. For example, some nerve entrapments, vitamin deficiencies, or even certain infections can cause muscle weakness or twitching. Tests to rule out other conditions or help. This process ensures that the diagnosis of ALS is made with as much certainty as possible, rather than jumping to conclusions.
These "rule-out" tests might include blood tests to check for various markers, or perhaps imaging scans like an MRI of the brain or spinal cord. The goal is to systematically eliminate other possibilities until the picture becomes clearer. This can sometimes make the diagnostic period feel long, but it's a necessary part of getting an accurate understanding of what's going on with your health, you know.
Understanding the Tests
While specific tests for ALS don't exist in the same way a blood test confirms diabetes, there are several diagnostic tools that help build the case for an ALS diagnosis. These tests assess the function of your nerves and muscles. For instance, one common test is electromyography (EMG), which measures the electrical activity of muscles. Another is nerve conduction study (NCS), which checks how well electrical signals are traveling along your nerves. These tests can show patterns of muscle and nerve damage consistent with ALS.
Doctors might also perform a muscle biopsy, though this is less common, or a lumbar puncture (spinal tap) to examine the cerebrospinal fluid. The combination of these test results, along with the neurologist's clinical observations and the progression of symptoms, is what ultimately leads to an ALS diagnosis. It's a comprehensive approach that explores how Amyotrophic Lateral Sclerosis, often called Lou Gehrig's disease, is diagnosed, and helps to learn about the team and tests that accurately detect ALS.
The Progression of Symptoms
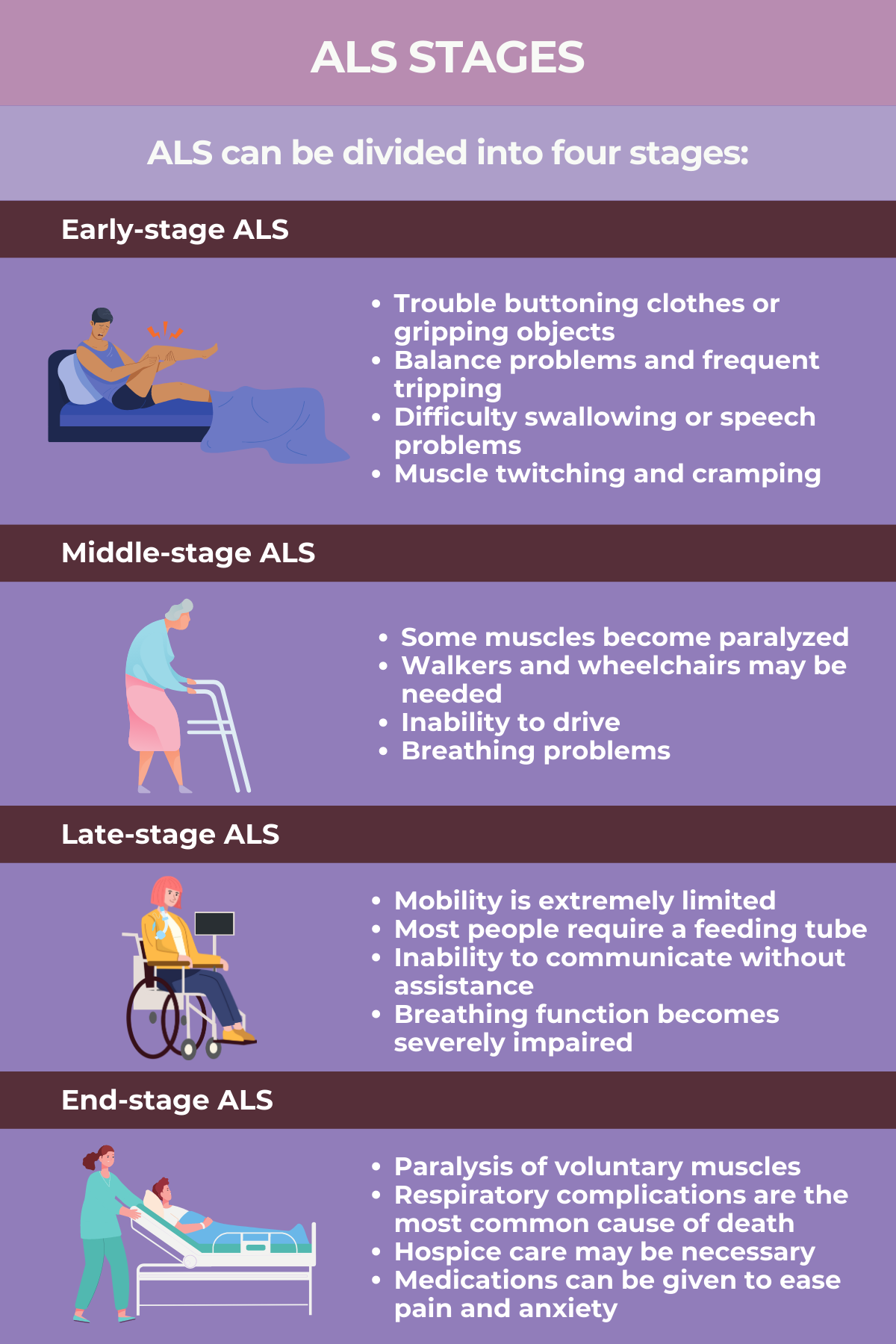
ALS is a progressive disease, which means its symptoms tend to get worse over time. What might start as a subtle weakness or twitch in one area can gradually spread to other parts of the body. Understanding this progression is a key part of the diagnostic process and helps doctors confirm the condition. It's a sad reality, but knowing what to expect can also help with planning for care.
From Early Signs to Broader Impact
As mentioned, ALS often begins with muscle twitching and weakness in a limb, or sometimes slurred speech. But as the disease moves forward, its effects become more widespread. Over time, movement, speech, chewing and swallowing, and breathing are all affected. The muscle weakness that gets worse can make simple tasks incredibly challenging. It's a gradual loss of control, which can be very difficult for individuals and their families to experience.
The progressive degeneration of nerve cells in the spinal cord and brain means that the signals to the muscles become weaker and weaker. This leads to a continuous decline in muscle function. It's a condition where, you know, the impact broadens from just one limb to affecting nearly all voluntary muscle movements. This pattern of worsening symptoms is a significant indicator for doctors when considering an ALS diagnosis.
Impact on Daily Life
As the disease progresses, the complications from ALS can become quite significant. For instance, during the worsening of the disease, Amyotrophic Lateral Sclerosis (ALS) causes complications such as difficulty breathing, problems with eating and swallowing, and an increased risk of falls due to muscle weakness. These challenges mean that daily activities that most people take for granted, like getting dressed or even just talking, can become very hard to manage.
Eventually, ALS affects control of the muscles needed to move, speak, eat and breathe. This means that people with ALS will eventually need assistance with many aspects of their daily lives. The impact on quality of life is profound, and this is why early and accurate diagnosis is so important, allowing for planning and support systems to be put into place as soon as possible. It's about facing a challenging future with as much preparation and support as possible.
Frequently Asked Questions About ALS Diagnosis
People often have many questions when thinking about an ALS diagnosis. Here are some common ones:
Is ALS hard to diagnose early?
Yes, it can be quite hard to diagnose ALS early on. This is because its initial symptoms, such as tripping or dropping things, are often similar to those of many other conditions. Doctors need to perform various tests to rule out these other possibilities before they can confirm an ALS diagnosis, which, you know, takes some time.
What kind of doctor diagnoses ALS?
While your primary care doctor might be the first to notice your symptoms, they will typically refer you to a neurologist for an ALS diagnosis. A neurologist is a doctor who has specialized training in diseases of the nervous system, including conditions like Amyotrophic Lateral Sclerosis. They are the experts who can really get to the bottom of what's happening with your nerves and muscles.
What are the very first signs of ALS?
The very first signs of ALS can vary, but they often include muscle twitching, especially in a limb, or a feeling of weakness in an arm or leg. Some people might also notice slurred speech or difficulty with swallowing. These early symptoms usually affect your extremities first, or sometimes, you know, your breathing and eating functions.
Looking Ahead After Diagnosis
An ALS diagnosis is a life-altering event, and it brings with it a need for comprehensive care and support. While there is currently no cure for ALS, treatments are available that can help manage symptoms and improve quality of life. The focus shifts to providing the best possible support for daily living and maintaining comfort. It's about finding ways to live as fully as possible with the condition.
Understanding the journey to an ALS diagnosis is just the beginning. It opens the door to connecting with specialized care teams and resources that can provide ongoing assistance. For more information about motor neuron diseases and how they affect the body, you can explore resources like the National Institute of Neurological Disorders and Stroke. Learn more about ALS and its management on our site, and for details on support services, you can also link to this page here. It's a path that requires courage and a strong support network, and knowing what to expect can make a big difference.
Detail Author 👤:
- Name : Mr. Heber Grant I
- Username : cummerata.rosalia
- Email : oschuster@luettgen.com
- Birthdate : 1999-03-06
- Address : 658 Merl Bridge Apt. 636 Walterborough, OK 57965-0421
- Phone : +1 (813) 798-6975
- Company : Murazik, Wolff and Kling
- Job : Designer
- Bio : Pariatur labore neque assumenda harum molestiae neque consectetur. Id odit aut non quaerat repellat dolorem maiores. Qui omnis ea consectetur laboriosam tenetur.
Socials 🌐
facebook:
- url : https://facebook.com/fay1987
- username : fay1987
- bio : Et earum expedita et velit optio.
- followers : 4546
- following : 1246
linkedin:
- url : https://linkedin.com/in/lfay
- username : lfay
- bio : Delectus consequatur fugit quaerat id corporis.
- followers : 3074
- following : 885
tiktok:
- url : https://tiktok.com/@leannfay
- username : leannfay
- bio : Fugit reprehenderit fuga mollitia ipsam tempora. Nemo tempore atque est sint.
- followers : 1328
- following : 1167
instagram:
- url : https://instagram.com/leannfay
- username : leannfay
- bio : In ut ipsam aut voluptatem. Neque voluptatem quae aut quod quo fugit mollitia.
- followers : 657
- following : 1030