Understanding A Pancreatic Attack: What You Need To Know
Feeling a sudden, sharp pain in your abdomen, perhaps radiating to your back? That could be a sign of a pancreatic attack, a condition that truly deserves your attention. It’s a moment when your pancreas, a vital organ tucked behind your stomach, becomes inflamed, and it can be quite serious. You might be wondering what exactly is happening inside your body when this occurs, and that's a good question to ask.
Pancreatitis, which is the medical term for this inflammation, can strike out of the blue, or it might build up over a period of time. This digestive system disorder, as you can imagine, is capable of causing significant illness, so knowing the symptoms and what might cause it becomes rather important. It's not something you want to ignore, you know, because early awareness can make a big difference.
Many people experience a form of pancreatitis that shows up quite suddenly, often called acute pancreatitis. Others might deal with a more persistent, long-term version. Understanding these different ways a pancreatic attack can show up, and what you can do about it, is truly the first step toward feeling better and protecting your health, especially if you've ever felt that kind of pain yourself.
- Nfl Superbowl Mvps
- What Day Did The Queen Of England Die
- Incredible Four Movie
- Olivia Newton
- Fergie Music Videos
Table of Contents
- What Exactly is a Pancreatic Attack?
- Recognizing the Signs: Symptoms of a Pancreatic Attack
- What Triggers These Attacks? Common Causes
- Getting a Diagnosis: Unraveling the Mystery
- Managing a Pancreatic Attack: Treatment and Care
- Living with Pancreatitis: Long-Term Outlook
- Frequently Asked Questions About Pancreatic Attacks
What Exactly is a Pancreatic Attack?
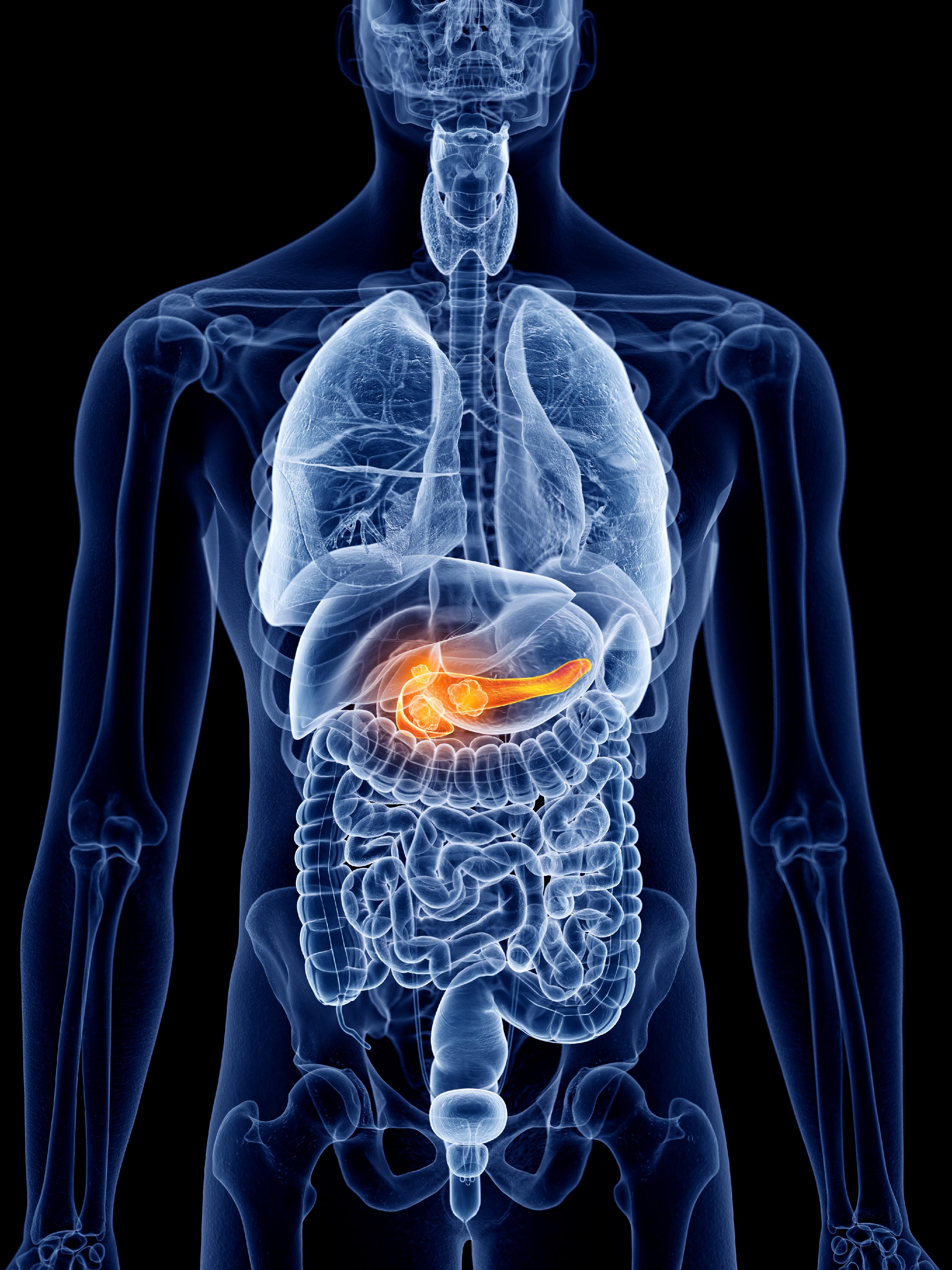
A pancreatic attack, or pancreatitis, happens when the pancreas becomes inflamed. This little organ, shaped kind of like a flat pear, sits behind your stomach and plays a big part in your digestion and blood sugar regulation. When it gets inflamed, its own digestive enzymes, which normally activate in your small intestine, actually start to activate inside the pancreas itself. This can cause quite a bit of irritation and damage, so it's a pretty serious situation.
It's interesting how this condition can vary so much from person to person. Some individuals might experience a relatively mild episode, while for others, it can be quite severe, requiring immediate medical attention. Knowing the different ways this inflammation can show up is really helpful, as a matter of fact, for recognizing what you might be dealing with.
Acute vs. Chronic Pancreatitis
Pancreatitis, you see, generally comes in two main forms: acute and chronic. The acute form is what most people experience, appearing quite suddenly. It’s a sudden onset of inflammation, often causing intense pain, and it can be a rather alarming event. Mild cases of acute pancreatitis can sometimes resolve on their own, or with minimal treatment, but it's always best to get it checked out.
Chronic pancreatitis, on the other hand, is a long-term condition. It develops over time, often after repeated bouts of acute pancreatitis, and it means there's ongoing damage to the pancreas. This can lead to persistent pain and problems with digestion, as the pancreas slowly loses its ability to function properly. It's a more challenging condition to manage, frankly, because the damage can accumulate over the years.
Autoimmune Pancreatitis: A Different Angle
There's also a specific type of pancreatitis called autoimmune pancreatitis. This is where your body's own immune system, which is supposed to protect you, mistakenly starts attacking the pancreas itself. It's a bit like your body gets confused and turns against its own healthy tissues, causing inflammation. This condition is also sometimes called IgG4-related disease, and it's a distinct form that requires its own specific approach to care.
Recognizing autoimmune pancreatitis is important because its treatment can be different from other forms of pancreatitis. It's a fascinating area of medicine, really, how the immune system can go awry in such specific ways. This particular type of pancreatic attack might require treatments that focus on calming down the overactive immune response, which is quite different from managing, say, gallstone-induced pancreatitis.
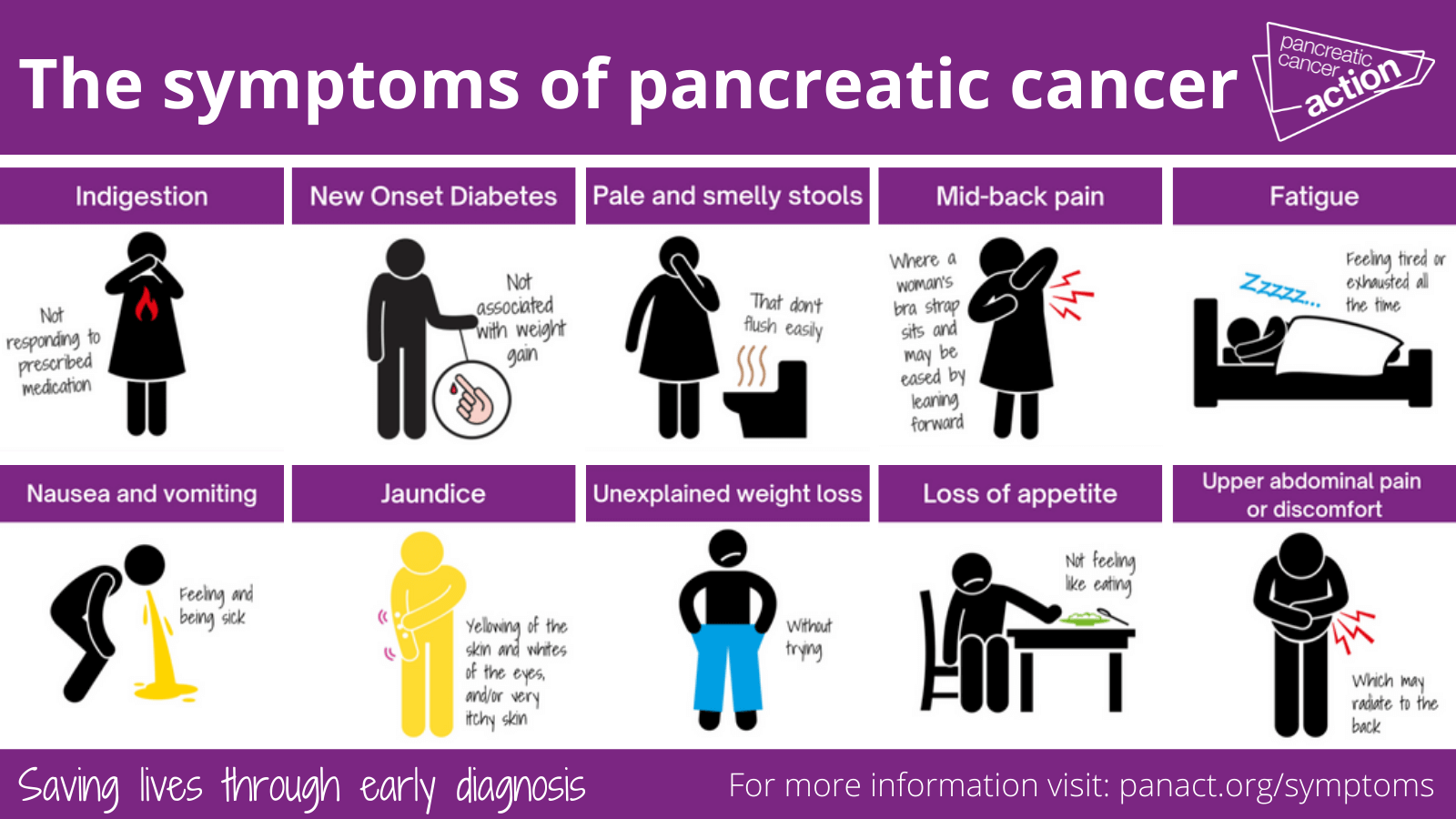
Recognizing the Signs: Symptoms of a Pancreatic Attack
Knowing the symptoms of a pancreatic attack is incredibly important for getting help quickly. The pain can be quite distinct, and it's often the first major clue that something is wrong. People describe it in various ways, but there are some common patterns that tend to show up. It’s not just a general stomach ache; it often has a very specific feel to it, you know.
The symptoms can range from mild discomfort to severe, debilitating pain. Sometimes, they might even mimic other conditions, which can make diagnosis a bit tricky at first. However, paying close attention to where the pain is and how it feels can provide valuable information for your doctor, and that's pretty much always a good idea.
Where Does the Pain Hit?
One of the most characteristic symptoms of a pancreatic attack is pain that spreads across your back. It can feel quite similar to the discomfort you might experience with a gallbladder issue or another type of pancreatitis attack. For some, this pain isn't just in the back; it can also be referred pain, meaning it travels to other areas, like up to your shoulder. This radiating pain is a key indicator, apparently, that your pancreas might be the source of the trouble.
The location and nature of the pain can be quite specific, so it's not just a general tummy ache. It might be a constant, dull ache, or it could be a sharp, stabbing sensation. What's more, the pain often gets worse after eating, especially fatty foods, and can be aggravated by lying down or lying back soon after a meal. This particular detail, as I was saying, is something many people notice and report to their doctors.
Digestive Distress and Other Clues
Beyond the pain, a pancreatic attack can bring on a host of digestive problems. You might experience nausea, vomiting, and a tender abdomen. These symptoms are your body's way of telling you that something is off with your digestive process. The pancreas is so central to breaking down food, that when it's inflamed, digestion really struggles, you know.
In chronic pancreatitis, specifically, people often deal with persistent stomach pain and cramping. One individual mentioned being prescribed Creon, which are digestive enzymes, and finding that they relieved the stomach pain, cramping, and digestion portion of their symptoms. This highlights how important those enzymes are for proper digestion, and how their absence or malfunction can cause significant discomfort. It's a pretty clear sign, actually, that the pancreas isn't doing its job right.
What Triggers These Attacks: Common Causes
Understanding what can cause a pancreatic attack is a really important step in preventing future episodes or managing the condition effectively. There are several common culprits, and sometimes, it can be a combination of factors. It’s not always straightforward, but doctors have identified some key triggers that show up quite often, and that's good to know, you know, for prevention.
For instance, some causes are related to blockages, while others involve the body's own immune system. Knowing these distinctions can help guide treatment and lifestyle changes. It’s fascinating, in a way, how different things can lead to the same kind of inflammation in the pancreas, but they do.
The Role of Gallstones
Gallstones are a very common cause of pancreatitis. These small, hard deposits form in your gallbladder, which is a little organ that stores bile. Sometimes, these gallstones can slip out of the gallbladder and block the bile duct. This duct is shared by both the gallbladder and the pancreas, and when it gets blocked, pancreatic enzymes can't travel to the small intestine where they're supposed to go. Instead, they get backed up and start to activate inside the pancreas, causing inflammation. It’s a pretty direct cause-and-effect, honestly, when gallstones are involved.
This blockage essentially creates a traffic jam for digestive fluids, leading to the pancreatic attack. It's a situation where a small stone can cause a really big problem for a vital organ. If you have gallstones, your doctor might discuss options to prevent them from causing future pancreatitis episodes, which is definitely something to consider.
When Your Own Body Attacks
As mentioned earlier, autoimmune pancreatitis occurs when your immune system, for reasons not fully understood, decides to attack your pancreas. This is a case where your body's defense mechanisms turn against itself, causing inflammation and damage. It’s a complex process, but it basically means your immune cells are targeting the pancreatic tissue as if it were a foreign invader. This can be a rather puzzling situation, you know, when your own body is the problem.
This type of attack is different from, say, a gallstone blockage because it stems from an internal misdirection of the immune system. Identifying if your pancreatitis is autoimmune is crucial because the treatment approach will focus on modulating the immune response, which is a very specific kind of therapy.
Lifestyle and Other Factors
Beyond gallstones and autoimmune issues, other factors can contribute to a pancreatic attack. For example, one person mentioned noticing pain if they eat at night and then lie down or lie back soon after. This suggests that certain eating habits combined with posture might aggravate the pancreas, potentially by causing digestive fluids to reflux or put pressure on the organ. It's a very specific observation, and it highlights how individual experiences can vary.
Alcohol consumption is another well-known risk factor for pancreatitis, especially chronic forms. High levels of triglycerides (a type of fat in the blood) can also trigger attacks. Certain medications, infections, and even abdominal injuries can lead to pancreatitis. It's a pretty wide range of potential causes, honestly, so a thorough medical evaluation is always a good idea.
Getting a Diagnosis: Unraveling the Mystery
When you're experiencing symptoms that suggest a pancreatic attack, getting a clear diagnosis is the next critical step. Doctors use a variety of tools and tests to figure out exactly what's going on inside your body. It's not always a simple process, as symptoms can overlap with other digestive issues, but modern medicine offers some really good ways to pinpoint the problem, and that's certainly reassuring.
The goal is to confirm inflammation of the pancreas, identify the cause, and assess the severity of the condition. This helps doctors create the most effective treatment plan for you. It's a bit like being a detective, gathering all the clues to solve the case, you know, for your health.
Modern Tools for Clear Answers
One valuable diagnostic tool is endoscopic ultrasound. This procedure involves a small tube with an ultrasound device on its tip, which is gently fed through your mouth and into your digestive system. It provides very detailed images of the pancreas and surrounding structures. This allows doctors to see inflammation, spot gallstones that might be causing blockages, look for signs of cancer, or identify other obstructions in the pancreatic ducts. It's a remarkably precise way to get a look at things, apparently.
Beyond imaging, blood tests are also crucial. They can measure levels of pancreatic enzymes like amylase and lipase, which are typically elevated during a pancreatic attack. Doctors also consider your medical history and the specific symptoms you're experiencing. There's even talk about how artificial intelligence is transforming patient outcomes in pancreatic conditions, especially when it comes to early diagnosis of more serious issues like pancreatic cancer. This kind of technology is really offering new hope, as a matter of fact, for quicker and more accurate diagnoses.
Managing a Pancreatic Attack: Treatment and Care
Once a pancreatic attack is diagnosed, the focus shifts to treatment and care. The approach varies significantly depending on whether it's an acute or chronic condition, and what caused it. The main goals are to reduce inflammation, manage pain, and prevent complications. It's a very individualized process, really, because every person's situation is a bit different.
For acute attacks, the immediate priority is usually supportive care to allow the pancreas to heal. For chronic conditions, the treatment is more about long-term management and symptom relief. It’s about helping your body recover and function as well as possible, you know, for your everyday life.
Easing the Pain and Aiding Digestion
For many, managing the pain is a primary concern during a pancreatic attack. Pain relievers are often prescribed to help cope with the discomfort. Beyond pain, digestive issues are common, especially in chronic pancreatitis. As one person mentioned, they were diagnosed with pancreatitis and found significant relief from stomach pain, cramping, and digestion problems after being prescribed Creon, which are digestive enzymes. These enzymes help your body break down food properly, taking some of the burden off your inflamed pancreas. It's pretty much a game-changer for digestion, honestly, when those enzymes are working.
Sometimes, doctors might recommend a temporary period of fasting to give the pancreas a rest, followed by a gradual reintroduction of clear liquids and then solid foods. This helps to reduce the stimulation of the pancreas and allows it to recover. It's a gentle approach, basically, to let the organ heal itself.
Serious Complications and Procedures
Acute pancreatitis can sometimes make the pancreas vulnerable to infections. Pancreatic infections are quite serious and demand intensive treatment, which might include surgery or other procedures to remove the infected tissue. This is why close monitoring by medical professionals is so important during an acute attack. It's a pretty critical situation, apparently, when an infection sets in.
In cases where pancreatic cancer is involved, or for certain severe chronic conditions, more complex procedures might be necessary. The Whipple procedure, for example, is a major surgery often used to treat pancreatic cancer, especially when the tumor is in the head of the pancreas. This is a complex operation that involves removing part of the pancreas, gallbladder, and portions of the small intestine. New technologies are actually improving pancreatic cancer treatment, offering hope to patients facing one of the least survivable forms of cancer. This progress is really quite significant, you know, in a challenging field.
Living with Pancreatitis: Long-Term Outlook
Living with pancreatitis, especially the chronic form, often means making ongoing adjustments to your lifestyle and working closely with your healthcare team. It's about finding ways to manage symptoms, prevent future attacks, and maintain your quality of life. It’s a journey that requires patience and a willingness to adapt, honestly, but it's certainly manageable for many.
Regular check-ups and open communication with your doctor are key. You might also find it helpful to consult with specialists, like a registered dietitian, especially if you've had surgery like the Whipple procedure. They can offer guidance on nutrition and help ensure you're getting the right nutrients. This kind of team approach is really important, you know, for comprehensive care.
Diet and Lifestyle Adjustments
Diet plays a huge role in managing pancreatitis. Eating a low-fat diet is often recommended to reduce the burden on the pancreas. Avoiding alcohol is almost always advised, as it's a major trigger for many. Small, frequent meals might be easier to digest than large ones, too. These adjustments can make a big difference in how you feel day-to-day and can help prevent flare-ups. It's about being mindful of what you put into your body, basically, to support your pancreas.
For someone who notices pain after eating at night and lying down, adjusting meal timing or posture after eating could be a simple yet effective lifestyle change. It's about listening to your body and understanding its unique responses to different habits. Every little bit helps, in some respects, when you're dealing with a sensitive organ like the pancreas.
The Connection to Other Conditions
Sometimes, pancreatitis can coexist with other health issues, or even be a symptom of a more serious underlying condition. For example, one person mentioned their doctor recently told them they have IBS, and they suspect they might have both IBS and chronic pancreatitis. This highlights how symptoms can overlap and how important it is to get a complete diagnosis to ensure you're being treated for all your conditions. It's definitely concerning not to be treated completely and risk further damage to your pancreas, so getting a full picture is vital.
It's also important to be aware of the connection between pancreatitis and pancreatic cancer. While most cases of pancreatitis are not cancer, chronic inflammation can sometimes increase the risk over time. Pancreatic cancer is a very aggressive and challenging cancer to diagnose and treat, but new technologies are improving treatment options. Early diagnosis, often aided by advanced imaging and even artificial intelligence, is incredibly important for better outcomes. You can learn more about pancreatic cancer from reliable sources like the National Cancer Institute. It's a serious topic, honestly, but staying informed is always a good thing.
Working with a multidisciplinary team of specialists, including oncologists, surgeons, and radiation specialists, is often part of creating a comprehensive treatment plan for pancreatic cancer. This team approach ensures that all aspects of the condition are addressed. It's a very thorough way to approach such a complex illness, you know, giving patients the best possible care.
Frequently Asked Questions About Pancreatic Attacks
Here are some common questions people ask about pancreatic attacks:
What does a pancreatic attack feel like?
A pancreatic attack often feels like a severe, sudden pain in the upper abdomen, which can spread to your back. It might be a constant, sharp ache, and sometimes, it can feel like referred pain up to your shoulder. Nausea, vomiting, and a tender belly are also common. The pain often gets worse after eating, especially fatty foods, and can be aggravated by lying down, you know, or lying back soon after a meal.
Can a pancreatic attack be mild?
Yes, mild cases of pancreatitis can occur. In some instances, the symptoms might be less severe, and the condition could even resolve on its own with supportive care. However, even mild symptoms should prompt a visit to a doctor to confirm the diagnosis and rule out more serious issues. It's always best to get it checked out, as a matter of fact, to be on the safe side.
How is a pancreatic attack diagnosed?
Doctors diagnose a pancreatic attack by looking at your symptoms, performing a physical examination, and conducting tests. Blood tests can check for elevated pancreatic enzymes like amylase and lipase. Imaging tests, such as endoscopic ultrasound, CT scans, or MRIs, can show inflammation, gallstones, blockages, or other abnormalities in the pancreas. This combination of information helps confirm the diagnosis and identify the underlying cause, which is pretty much essential for proper treatment.
Learn more about pancreatitis on our site, and link to this page here for more specific treatment information.

Detail Author 👤:
- Name : Dr. Meghan Gottlieb
- Username : gunner28
- Email : adamore@hotmail.com
- Birthdate : 1978-02-28
- Address : 715 Jace Vista Suite 870 Lake Stephanview, NY 25515-9850
- Phone : +15674778824
- Company : Toy-Veum
- Job : Medical Assistant
- Bio : Fuga magni sit dolorem omnis. Delectus temporibus consequuntur ratione ut laboriosam consequatur a et. Minus quas sint culpa.
Socials 🌐
instagram:
- url : https://instagram.com/elizametz
- username : elizametz
- bio : Est adipisci voluptatem quidem eaque. Unde et fugit excepturi suscipit cum atque.
- followers : 5051
- following : 505
linkedin:
- url : https://linkedin.com/in/eliza4564
- username : eliza4564
- bio : Voluptas quae praesentium quaerat saepe at.
- followers : 5931
- following : 2241
facebook:
- url : https://facebook.com/metze
- username : metze
- bio : Id laudantium eos hic deserunt sed sunt. Nulla labore aut sed sapiente sunt.
- followers : 477
- following : 1520
tiktok:
- url : https://tiktok.com/@elizametz
- username : elizametz
- bio : Eos hic molestias est libero magni molestiae exercitationem sed.
- followers : 777
- following : 295
twitter:
- url : https://twitter.com/metz1993
- username : metz1993
- bio : Repellat officiis quia enim eos quo ducimus. Quisquam quam sunt quia ratione voluptas neque. Rerum provident aut quaerat id et velit aut dolores.
- followers : 3830
- following : 1821