Understanding Diabetes Type 1 Insulin: Your Guide To Managing Life
Living with type 1 diabetes can feel like a big challenge, especially when you first hear the news, and it's a condition that truly impacts too many people and their loved ones. The American Diabetes Association, for instance, is actively fighting back with important research, education, and advocacy, and they are not stopping until everyone has the tools they need. This chronic illness, known formally as diabetes mellitus, affects more than 37 million Americans, which is about one out of every ten people, so it's a condition many folks are dealing with.
You might feel a bit overwhelmed right now, trying to make sense of everything you need to know about diabetes, including its different types, what signs to look for, what causes it, and any risk factors. Learning about how it's diagnosed, and whether it can be, well, you know, reversed or cured, is often on people's minds. For type 1 diabetes, there isn't a cure or a way to reverse it, but it's absolutely something that can be managed with the right care, and that care often centers around insulin.
This article aims to shed some light on what diabetes type 1 insulin means for you or someone you care about. We will explore why it's so important, how it works, and some practical ways to live well with it every day. It's truly about giving you the information and resources you might need to manage this condition, so you can feel more in control.
Table of Contents
- What is Type 1 Diabetes and Why Insulin is Key
- How Insulin Works for People with Type 1 Diabetes
- Different Types of Insulin Used in Type 1 Diabetes
- Ways to Get Insulin into Your Body
- Daily Life with Diabetes Type 1 Insulin Management
- Living a Full Life with Type 1 Diabetes
- Common Challenges and Helpful Tips
- The Future of Diabetes Type 1 Insulin Management
- Frequently Asked Questions About Diabetes Type 1 Insulin
What is Type 1 Diabetes and Why Insulin is Key
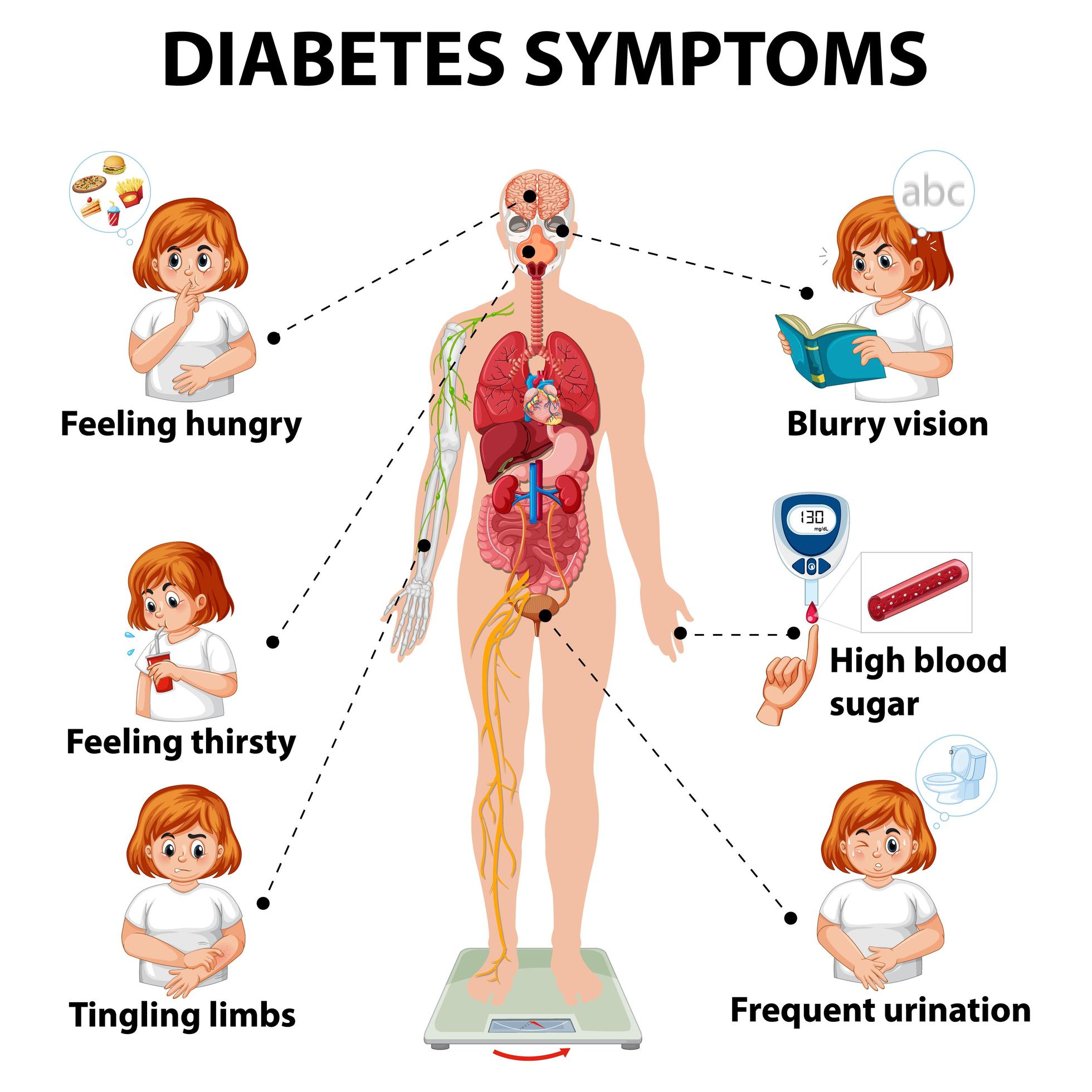
Diabetes, you see, occurs when your blood glucose, or blood sugar, is too high, and this can lead to various health problems. There are three main types of diabetes: type 1, type 2, and gestational. Type 1 diabetes is a chronic condition, meaning it stays with you, and it's a bit different from the others because your body just doesn't make insulin at all, or it makes very, very little.
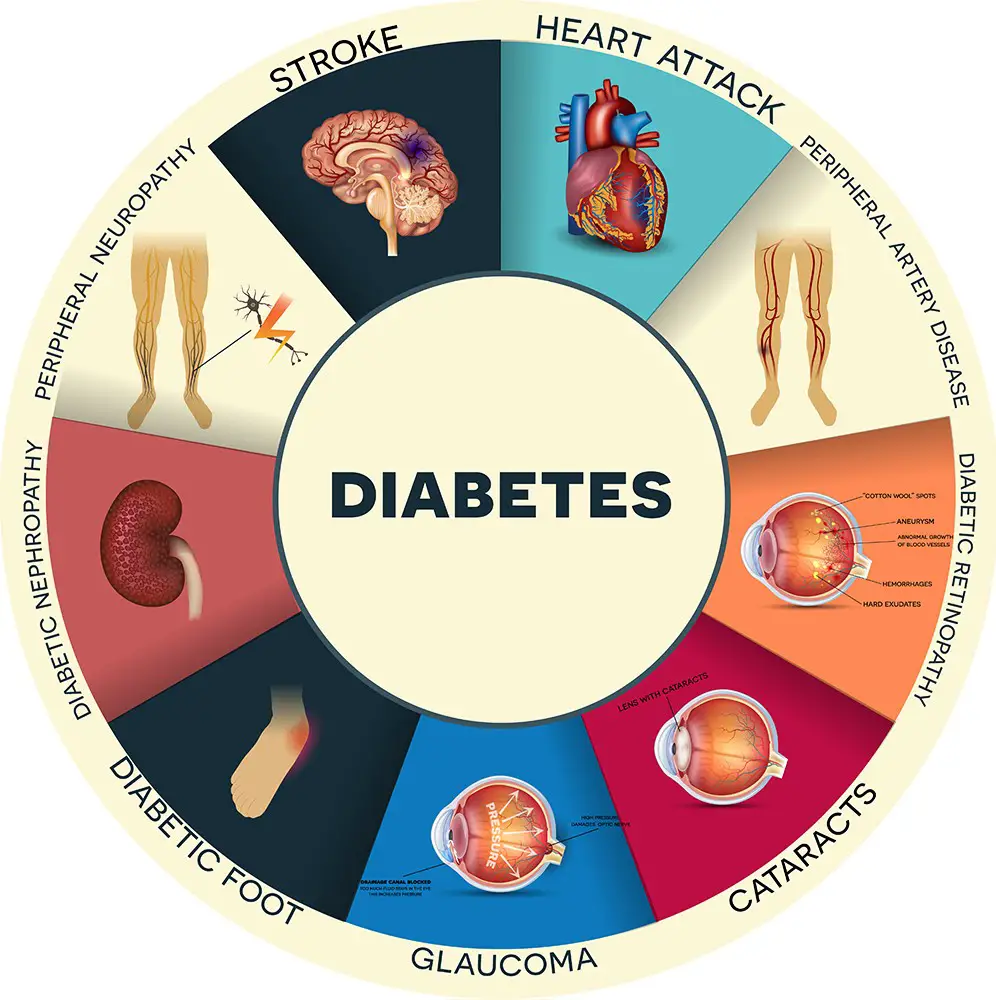
Insulin is a hormone that your body naturally produces, and it's really important because it helps glucose from the food you eat get into your cells. Once inside your cells, glucose can be used for energy. Without insulin, glucose just stays in your bloodstream, and that's when blood sugar levels become too high. This high blood sugar, over time, can quietly damage your eyes, heart, and kidneys for years without you even knowing, as diabetes often does not show signs early on.
For people with type 1 diabetes, taking insulin is not just a treatment; it's absolutely necessary for survival. It replaces the insulin your body can't make, allowing your cells to get the energy they need and keeping your blood sugar levels in a healthier range. This is why understanding diabetes type 1 insulin is so crucial.
How Insulin Works for People with Type 1 Diabetes
Think of insulin as a key, if you will. Your body's cells have little locks on them, and glucose, the sugar from your food, wants to get inside. Insulin is that key that unlocks the cell doors, letting the glucose in. Once glucose is inside the cells, it can be used for energy, which is pretty vital for everything your body does, from thinking to running.
With type 1 diabetes, your body's immune system, which usually fights off germs, mistakenly attacks and destroys the cells in your pancreas that make insulin. So, there are no keys being made, or almost none. This means the glucose stays locked out of your cells and builds up in your blood. That's why taking insulin from an outside source is so important; it provides those missing keys.
When you take insulin, it travels through your bloodstream to your cells, where it helps open those doors for glucose. This helps bring your blood sugar down to a safer level. It's a continuous balancing act, you see, trying to match the amount of insulin you take with the food you eat and the activity you do, so your blood sugar stays stable.
Different Types of Insulin Used in Type 1 Diabetes
Not all insulin is the same, which is interesting, and there are several types, each working a little differently. They are generally grouped by how quickly they start working, when they reach their peak effect, and how long they last in your body. This variety allows for a more personalized approach to managing blood sugar.
Rapid-Acting Insulin: This type starts working very quickly, usually within 15 minutes of taking it. It peaks in about an hour and lasts for two to four hours. People often take this right before or after a meal to cover the carbohydrates they're about to eat. It's really quite fast-acting.
Short-Acting (Regular) Insulin: This insulin takes a bit longer to start working, usually 30 minutes to an hour. Its peak effect is typically two to three hours after injection, and it can last for three to six hours. This is also taken before meals, but with a bit more planning.
Intermediate-Acting Insulin: This type starts working in about two to four hours, peaks in four to twelve hours, and can last for twelve to eighteen hours. It's used to cover blood sugar levels for a longer period, often taken twice a day.
Long-Acting Insulin: This insulin starts working slowly, usually within a few hours, and provides a steady, continuous release of insulin for up to 24 hours or even longer, with no significant peak. It's often called "basal" insulin because it provides a constant background level of insulin, keeping blood sugar stable between meals and overnight.
Ultra Long-Acting Insulin: Some newer insulins last even longer, sometimes up to 42 hours, offering even more flexibility and fewer injections for some people. This is a fairly new development.
Often, people with type 1 diabetes use a combination of these insulins. For example, they might use a long-acting insulin once or twice a day for their baseline needs and then use rapid-acting insulin with meals to cover the carbohydrates. This approach tries to mimic how a healthy pancreas would release insulin throughout the day.
Ways to Get Insulin into Your Body
Getting insulin into your body can be done in a few different ways, and the choice often depends on personal preference, lifestyle, and what works best for managing blood sugar levels. Each method has its own set of considerations, too, it's almost a personal choice.
Syringes and Vials: This is the traditional method. You draw insulin from a small bottle (vial) into a syringe and then inject it under your skin. It's a very precise way to measure your dose, and many people still use this method because it's reliable and straightforward.
Insulin Pens: These are pre-filled devices, or ones where you insert an insulin cartridge, that look a bit like a pen. They are very convenient and discreet. You dial up the dose you need, attach a small needle, and inject. They're often preferred for their ease of use, especially when you're out and about, you know.
Insulin Pumps: An insulin pump is a small, computerized device that delivers insulin continuously throughout the day through a tiny tube (catheter) inserted under your skin, typically in your abdomen. It provides a steady background (basal) insulin dose and allows you to deliver extra doses (boluses) for meals or to correct high blood sugar. This offers a lot of flexibility and can help keep blood sugar levels very stable, as a matter of fact.
Smart Insulin Pens: These are newer devices that connect to smartphone apps. They can track your insulin doses, help with dose calculations, and even integrate with continuous glucose monitors. They offer a bit more technology to help manage your condition, which is pretty neat.
The best method for you is something you'd discuss with your healthcare team. They can help you figure out what fits your daily routine and helps you manage your blood sugar most effectively, really.
Daily Life with Diabetes Type 1 Insulin Management
Managing type 1 diabetes with insulin is truly an ongoing process, a bit like a daily dance, if you will. It involves several key practices to keep blood sugar levels in a healthy range and avoid complications. It's about being aware and making informed choices, basically.
Keeping an Eye on Blood Sugar Levels
Regularly checking your blood sugar is absolutely fundamental to managing type 1 diabetes. This helps you understand how your body responds to food, activity, and insulin doses. There are two main ways people do this.
Fingerstick Blood Glucose Meters: This involves pricking your finger to get a small drop of blood, which you then place on a test strip that goes into a meter. The meter gives you a blood sugar reading almost instantly. You'll typically check several times a day, before and after meals, before bed, and sometimes overnight.
Continuous Glucose Monitors (CGMs): A CGM is a small sensor inserted under your skin, usually on your arm or abdomen, that measures glucose levels in the fluid between your cells every few minutes. It sends these readings wirelessly to a receiver or a smartphone app. CGMs provide a much more complete picture of your blood sugar trends, showing highs, lows, and how your levels change throughout the day and night. This can be incredibly helpful for making real-time decisions about insulin doses, you know.
Knowing your blood sugar numbers is like having a map; it tells you where you are and helps you decide where you need to go with your insulin. This information is critical for making adjustments, frankly.
Understanding Carbohydrates and Insulin Doses
For people with type 1 diabetes, counting carbohydrates is a very important skill. Carbohydrates are the main nutrient in food that affects blood sugar levels. When you eat carbs, they break down into glucose, which then enters your bloodstream.
To manage this, you learn to calculate how many grams of carbohydrates are in your meals and snacks. Based on this, and your individual insulin-to-carb ratio, you determine how much rapid-acting insulin you need to take. This ratio is unique to each person and can even change throughout the day. For example, if your ratio is 1 unit of insulin for every 10 grams of carbs, and you eat a meal with 50 grams of carbs, you would take 5 units of insulin. It's a bit of math, but it becomes second nature.
This precise matching of insulin to carbohydrates helps prevent blood sugar spikes after eating. It allows for much more flexibility in what you eat, which is pretty important for a normal life, as a matter of fact.
Managing Insulin During Illness
When you're sick, managing type 1 diabetes can become a bit more complicated. Illness, even a common cold, can cause your blood sugar levels to rise, sometimes quite significantly. Your body releases stress hormones when it's fighting an infection, and these hormones can make your cells more resistant to insulin.
During sick days, you might need more insulin than usual, even if you're not eating much. It's important to continue taking your insulin, never stop it, and to monitor your blood sugar levels more frequently. You also need to watch for signs of diabetic ketoacidosis (DKA), a serious complication that can happen when there's not enough insulin in your body.
Having a "sick day plan" developed with your healthcare team is really helpful. This plan usually includes guidelines for checking blood sugar and ketones, adjusting insulin doses, and knowing when to call for medical help. Staying hydrated is also key during these times, you know.
Living a Full Life with Type 1 Diabetes
Having type 1 diabetes doesn't mean you can't live a full, active, and happy life. It just means you have to be a bit more mindful about certain things. Many people with type 1 diabetes participate in sports, travel, pursue careers, and raise families, which is really quite inspiring.
Regular physical activity is very beneficial for managing blood sugar, but it does require careful planning with insulin doses and carbohydrate intake to prevent low blood sugar (hypoglycemia). Exercise can make your body more sensitive to insulin, so you might need less insulin on days you're more active.
Eating a balanced diet is also important. While carb counting allows for flexibility, choosing nutritious foods supports overall health. Working closely with your diabetes care team, including a dietitian, can help you create a meal plan that fits your lifestyle and helps you manage your blood sugar well.
Support groups and connecting with other people who have type 1 diabetes can also be incredibly helpful. Sharing experiences and tips can make you feel less alone and provide practical advice. It's good to know you're not the only one dealing with this, you know.
Common Challenges and Helpful Tips
Even with the best management, there will be days that are a bit tougher than others. Blood sugar levels can be unpredictable, affected by stress, hormones, illness, and even weather changes. It's a bit of a moving target, sometimes.
Hypoglycemia (Low Blood Sugar): This happens when your blood sugar drops too low, usually from too much insulin, not enough food, or too much activity. Symptoms can include shakiness, sweating, confusion, and dizziness. It's important to treat low blood sugar quickly by consuming fast-acting carbohydrates like glucose tablets, juice, or regular soda. Always carry these with you, basically.
Hyperglycemia (High Blood Sugar): This is when your blood sugar is too high, often from not enough insulin, too many carbs, or illness. Symptoms can include increased thirst, frequent urination, and fatigue. Correcting high blood sugar usually involves taking more insulin, as advised by your doctor, and drinking plenty of water.
Burnout: Managing a chronic condition like type 1 diabetes can be mentally and emotionally draining. It's okay to feel overwhelmed sometimes. Recognizing signs of burnout and seeking support from your healthcare team, friends, or family is very important. Remember that you're doing a lot, and it's okay to ask for help, you know.
The key is to learn from these experiences and adjust your management plan with your healthcare provider. Every day is a learning opportunity, truly.
The Future of Diabetes Type 1 Insulin Management
The world of diabetes research is always moving forward, which is very encouraging. There's a lot of exciting work happening right now, like the discussions at the 3rd International Conference on Diabetes, which is scheduled for Sunday, July 13, 2025. Researchers are always looking for better ways to manage the condition, and even for a cure, which is the ultimate goal.
New technologies are constantly being developed to make insulin delivery and blood sugar monitoring easier and more effective. For instance, there's ongoing work on "closed-loop" systems, sometimes called artificial pancreases. These systems combine an insulin pump with a continuous glucose monitor and a computer algorithm to automatically adjust insulin delivery based on real-time blood sugar readings. This could significantly reduce the burden of daily management for many people, which is pretty exciting.
There's also research into new forms of insulin, different ways to deliver it, and therapies that might help preserve the remaining insulin-producing cells in people newly diagnosed with type 1 diabetes. The American Diabetes Association, as mentioned, is fighting back with research and advocacy, and they are not stopping until breakthroughs make a huge difference. This constant innovation offers a lot of hope for an even brighter future for those living with type 1 diabetes, you know.
Frequently Asked Questions About Diabetes Type 1 Insulin
Here are some common questions people often ask about diabetes type 1 insulin:
1. What exactly is the role of insulin in type 1 diabetes?
Insulin's role in type 1 diabetes is really about replacing what your body can no longer make. Since your pancreas stops producing insulin, you have to take it from an outside source. This insulin acts like a key, helping glucose from your food get into your cells to be used for energy, which keeps your blood sugar levels from getting too high, basically. It's absolutely vital for survival and managing the condition.
2. How often do people with type 1 diabetes need to take insulin?
The frequency of insulin injections or pump delivery for type 1 diabetes varies, but it's typically multiple times a day. Most people use a combination of long-acting insulin, which provides a steady background dose, often once or twice a day, and rapid-acting insulin, which is taken with meals and snacks to cover carbohydrates. So, it's usually several times a day, sometimes more, depending on your individual needs and management plan, you know.
3. Can type 1 diabetes be cured with insulin?
No, unfortunately, type 1 diabetes cannot be cured with insulin. Insulin is a life-saving treatment that helps manage the condition by replacing the insulin your body can't make. While it's incredibly effective at controlling blood sugar levels and allowing people to live healthy lives, it doesn't address the underlying autoimmune process that destroys the insulin-producing cells. So, while it's managed with the right care, type 1 diabetes can't be reversed or cured, as a matter of fact.
For more general health information, you might find resources from the National Institute of Diabetes and Digestive and Kidney Diseases helpful.
:max_bytes(150000):strip_icc()/glucose-level-blood-test-1185738340-75b803e23e9a4ce6a550cbf41c3c2972.jpg)
Detail Author 👤:
- Name : Karlee Zieme
- Username : jodie.hintz
- Email : rowena.bartoletti@hotmail.com
- Birthdate : 2007-01-17
- Address : 5463 Barton Ridges Suite 344 New Elda, IA 25396-8956
- Phone : 352-640-2247
- Company : Weber-Daniel
- Job : Alteration Tailor
- Bio : Amet dolor sit rerum doloremque excepturi magni. Recusandae enim officiis similique et accusamus accusamus. Fugiat minus assumenda ut et. Repudiandae sed sed nemo id qui ut.
Socials 🌐
twitter:
- url : https://twitter.com/shanna.emard
- username : shanna.emard
- bio : Animi rem nisi perspiciatis expedita atque minima. Facilis magnam enim doloremque aperiam sed. Provident perspiciatis nemo magnam pariatur.
- followers : 1881
- following : 753
instagram:
- url : https://instagram.com/shanna_emard
- username : shanna_emard
- bio : Expedita maiores repudiandae et magnam. Provident eius eos labore sed culpa aliquam non amet.
- followers : 544
- following : 235